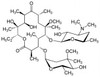
Clarithromycin, USP is a macrolide antibiotic that is a derivative of Erythromycin. This compound, developed in 1980, is both a substrate and inhibitor of CYP3A4. Clarithromycin has anti-cancer properties. Clarithromycin-related compounds are also available as highly pure EvoPure® products.
Clarithromycin is slightly soluble in aqueous solution.
Clarithromycin, USP conforms to United States Pharmacopeia specifications.
We also offer:
- Clarithromycin ReadyMadeTM Solution (C288)
- Clarithromycin related compound C, EvoPure® (C128)
- Clarithromycin related compound D, EvoPure® (C140)
- Clarithromycin related compound H, EvoPure® (C143)
- Clarithromycin related compound I, EvoPure® (C131)
- Clarithromycin related compound J, EvoPure® (C132)
- Clarithromycin related compound K, EvoPure® (C133)
- Clarithromycin related compound L, EvoPure® (C134)
- Clarithromycin related compound M, EvoPure® (C133)
- Clarithromycin related compound Z, EvoPure® (E022)
| Mechanism of Action |
Macrolide antibiotics inhibit bacterial growth by targeting the 50S ribosomal subunit preventing peptide bond formation and translocation during protein synthesis. Resistance to Clarithromycin is commonly attributed to mutations in 50S rRNA preventing Clarithromycin binding allowing the cell to synthesize error-free proteins. It can also act as a negative allosteric modulator of the GABAA receptor. Anti-cancer mechanisms include reduction of cytokines, inhibition of autophagy, and anti-angiogenesis. The compound can act on signal transduction pathways, transcription factors, drug pharmacokinetics, growth signals, and metastasis. These features can be exploited to make tumor cells more prone to apoptosis and reduce escape mechanisms. The mechanism used depend on the type of cancer. |
| Spectrum | Clarithromycin is a broad-spectrum antibiotic with bacteriostatic action wide range of Gram-positive and Gram-negative bacteria including anaerobes. It is also effective for Mycoplasma and Mycobacteria. |
| Microbiology Applications | Clarithromycin is commonly used in clinical in vitro microbiological antimicrobial susceptibility tests (panels, discs, and MIC strips) against Gram-positive and Gram-negative microbial isolates. Medical microbiologists use AST results to recommend antibiotic treatment options.
Representative MIC values include:
Clarithromycin (TOKU-E) used in methacrylate-based copolymer films that released the compound (along with doxycycline and rifampicin) for up to 21 days were found to prevent biofilm formation when used in an in vitro bioreactor model (Rose et al, 2015). |
| Eukaryotic Cell Culture Applications | An in vitro study on the inhibitory effect of Clarithromycin on transporter-expressing HEK-293 cell lines or membrane vesicles with 13 transporters (OATP1B1, OATP1B3, OAT1, OAT3, OCT1, OCT2, MATE1, MATE2-K, P-gp, BCRP, MRP2, MRP3, and BSEP) found that inhibition profiles were unique to the transporter (Vermeer et al, 2016). Macrolide antibiotics exert anti-inflammatory effects through inhibition of the production of proinflammatory cytokines. Nuclear factor kb (NF-kb) is an important transcription factor for genes that encode proinflammatory cytokines. In vitro studies with human monocytic leukemia cell line U-937, human T-cell leukemia (Jurkat), a pulmonary epithelial cell line A549, and peripheral blood mononuclear cells were conducted. Clarithromycin was found to suppress the production of proinflammatory cytokines via inhibition of NF-kb (Ichiyama T et al, 2001). Clarithromycin can have immunomodulatory activity on human lymphocyte function. The compound suppressed the synthesis of IL-1a, IL-1b, TNF-a, and GM-CSF in a concentration-dependent manner. This suggests Clarithromycin may modify the acute-phase inflammatory response by disturbing the cytokine cascade (Morikawa K et al, 1996). |
| Cancer Applications | Clarithromycin is involved in autophagy-lysosome pathway. It can inhibit autophagy in myeloma and myeloid leukaemia cells. It inhibits lysosomal function after fusion of the autophagosomes with the lysosomes. Thus, it could be a potential adjuvant where autophagy is used by the tumor as an escape mechanism (Nakamura et al, 2010). The combined action of Clarithromycin with the proteasome inhibitor bortezomib enhances cytotoxicity in the breast cancer cell lines MDA-MB-231 and MDA-MB-468. A wild-type murine embryonic fibroblast (MEF) cell line also exhibited enhanced cytotoxicity (Komatsu et al, 2012). Direct antineplastic effects of CAM may depend on the tumor type. Researchers found a direct anti-tumor activity of CAM on lymphoma cells (Ochi et al, 2006) and it directly induced apoptosis in a murine B cell lymphoma cell line (Ohara et al, 2004). |
| Storage Conditions | ≤ 30 °C |
| Impurities | Any related compound: ≤1.0% Number of related compounds exceeding 0.4%: ≤ 4 Total Impurities: ≤ 3.5% |
| References |
Goldman RC, Zakula D, Flamm R, Beyer J, Capobianco J (1994) Tight binding of Clarithromycin, its 14-(R)-hydroxy metabolite, and erythromycin to Helicobacter pylori ribosomes. Antimicrob. Agents Chemother. 38(7):1496-500. PMID 7979278
Takahashi T et al (2018) Advances in pharmaceutical treatment options for narcolepsy. Exp. Opin. Orphan Drugs 6(10):597-610 Tenson T, Lovmar M and Ehrenberg M (2003) The mechanism of action of macrolides, lincosamides and streptogramin B reveals the nascent peptide exit path in the ribosome. J. Mol. Biol. 330(5):1005-1014 PMID 12860123 |
| MIC | Bacillus subtilis (PCI219)| 0.1|| Bacteroides fragilis| 0.016 - >32|| Bacteroides tectum | 0.125|| Bacteroides ureolyticus| 0.125 - 4|| Bilophila wadsworthia| 4 - 32|| Borrelia afzelii| 0.0019 - 0.0312|| Borrelia bissettii| 0.0078|| Borrelia burgdorferi| 0.0156 - 0.008|| Borrelia garinii| 0.0019 - 0.0312|| Borrelia valaisiana| 0.0039|| Brevibacterium spp.| ≤0.03 - >128|| Burkholderia mallei| 4 - 16|| Campylobacter coli| 0.03 - 128|| Campylobacter helveticus| 4|| Campylobacter jejuni| 0.03 - 128|| Chlamydia pneumonia| 0.015 - 0.125|| Chlamydia psittaci| 0.015|| Chlamydia trachomatis| 0.03|| Chlamydophila pneumonia| 0.015 - 0.06|| Clostridium clostridioforme| 0.125 - >32|| Clostridium difficile| 0.125 - 128|| Clostridium innocuum| 0.25 - >32|| Clostridium perfringens| 1|| Clostridium ramosum| 0.25 - >32|| Corynebacterium afermentans| 0.03 - >128|| Corynebacterium amycolatum| 0.06 - >128|| Corynebacterium jeikeium| ≤0.015 - >128|| Corynebacterium minutissimum| ≤0.015 - >64|| Corynebacterium pseudodiphtheriticum| ≤0.015 - 4|| Corynebacterium spp.| 0.008 - >64|| Corynebacterium striatum| ≤0.015 - >128|| Corynebacterium urealyticum| ≤0.015 - >64|| Coryneform| 0.03 - >128|| Edwardsiella hoshinae | 8 - 32|| Edwardsiella ictaluri | 4 - ≥128|| Edwardsiella tarda| 8 - 32|| Enterococci| ≤0.006 - ≥512|| Enterococcus faecalis| 1.56|| Enterococcus faecium| 1.56|| Enterococcus spp.| 0.12 - >128|| Erysipelothrix rhusiopathiae| 0.06|| Escherichia coli| 6.25 - >128|| Fusobacterium gonidiaformans | ≤0.015 - 32|| Fusobacterium mortiferum| 4 - >32|| Fusobacterium naviforme| ≤0.015 - 32|| Fusobacterium necrogenes | 4 - >32|| Fusobacterium necrophorum| ≤0.015 - 32|| Fusobacterium nucleatum| ≤0.015 - 32|| Fusobacterium russii | 2 - >32|| Fusobacterium ulcerans | 4 - >32|| Fusobacterium varium| >32|| Haemolytic streptococci| 0.015 - 16|| Haemophilus influenzae| 0.008 - >256|| Haemophilus spp.| 1 - 32|| Helicobacter bilis| 8|| Helicobacter mustelae| 1|| Helicobacter pullorum| 2|| Helicobacter pylori| ≤0.004 - 128|| Klebsiella pneumonia| 12.5|| Lactobacillus acidophilus| 1 - 10|| Lactobacillus gasseri | >100|| Lactobacillus johnsonii| 100|| Lactobacillus paracasei| >100|| Lactobacillus salivarius| 1|| Legionella adelaidensis| 0.012|| Legionella anisa| 0.032|| Legionella birminghamiensis| 0.125|| Legionella bozemanii| 0.024|| Legionella brunensis| 0.064|| Legionella cherrii| 0.032|| Legionella cincinnatiensis| 0.032|| Legionella dumofii| 0.025|| Legionella erythra| 0.125|| Legionella fairfieldensis| 0.012|| Legionella feeleii| 0.05|| Legionella geestiana| 0.064|| Legionella gormanii| 0.039|| Legionella gratiana| 0.032|| Legionella hackeliae| 0.06|| Legionella israelensis| 0.032|| Legionella jamestowniensis| 0.125|| Legionella jordanis| 0.125|| Legionella lansingensis| 0.048|| Legionella londiniensis| 0.032|| Legionella longbeachae| 0.087|| Legionella maceachernii| 0.06|| Legionella micdadei| 0.053|| Legionella moravica| 0.032|| Legionella nautarum| 0.032|| Legionella oakridgensis| 0.06|| Legionella pneumophila| 0.001 - 0.125|| Legionella quateirensis| 0.016|| Legionella quinlivanii| 0.032|| Legionella rubrilucens| 0.06|| Legionella sainthelensi| 0.046|| Legionella santicrucis| 0.046|| Legionella shakespearei| 0.064|| Legionella spiritensis| 0.032|| Legionella spp.| ≤0.004 - 0.12|| Legionella steigerwaltii| 0.016|| Legionella tucsonensis| 0.006|| Legionella wadsworthii| 0.032|| Legionella worsleiensis| 0.006|| Listeria monocytogenes| 0.06 - 0.125|| Listeria spp.| 0.12|| Moraxella catarrhalis| 0.008 - ≥64|| Morganella morganii| >100|| Mycobacteria | 32 - 64|| Mycobacterium abscessus| 0.06 - 64|| Mycobacterium africanum | 2.5 - 40|| Mycobacterium avium| 0.3 - >256|| Mycobacterium bovis | 0.07 - 40|| Mycobacterium chelonae| ≤0.03 - 2|| Mycobacterium fortuitum| ≥0.03 - >64|| Mycobacterium intracellulare| 4 - 12.5|| Mycobacterium marinum| 0.094 - 3|| Mycobacterium mucogenicum| ≤0.03 - 0.12|| Mycobacterium paratuberculosis | 0.15 - 2.5|| Mycobacterium peregrinum| 0.06 - 0.25|| Mycobacterium simiae | 5 - 40|| Mycobacterium smegmatis| >512|| Mycobacterium tuberculosis| 0.5 - 50|| Mycobacterium ulcerans | <0.125 -4|| Mycoplasma fermentans| 8 - >32|| Mycoplasma genitalium| ≤0.015 - 0.06|| Mycoplasma hominis| >32 - >64|| Mycoplasma hyopneumoniae| 16 - >64|| Mycoplasma penetrans| 0.12 - 0.25|| Mycoplasma pneumonia| 0.00048 - 0.25|| Neisseria cinerea| 0.5 - 4|| Neisseria lactamica| 2 - 4|| Neisseria meningitidis| 0.003 - 1|| Neisseria mucosa| 0.06 - 8|| Neisseria perflava| 0.25 - 16|| Neisseria polysaccharea| 0.007 - 1|| Neisseria sicca| 0.25 - 16|| Neisseria spp.| 1 - 10.015|| Oerskovia spp.| 0.03 - >128|| Pasteurella multocida| 0.39|| Peptostreptococcus anaerobius| 0.04|| Peptostreptococcus asaccharolyticus| 0.5 - >128|| Peptostreptococcus magnus| 0.5 - >32|| Peptostreptococcus micros| 0.5 - 0.6|| Peptostreptococcus prevotii| ≤0.015 - >32|| Pneumococci| 0.03 - 128|| Pneumococci| <0.016 - >128|| Porphyromonas asaccharolytica| ≤0.015 - >32|| Porphyromonas cangingivalis | 0.06 - 0.125|| Porphyromonas canoris | 0.06 - 0.125|| Porphyromonas cansulci | 0.06 - 0.125|| Porphyromonas circumdentaria | 0.06 - 0.125|| Porphyromonas gingivalis| 0.06 - 0.125|| Porphyromonas levii | 0.06 - 0.125|| Porphyromonas macacae | 0.06 - 0.125|| Prevotella bivia| 0.06 - >32|| Prevotella buccae| 0.06 - 1|| Prevotella denticola| 0.03 - 4|| Prevotella heparinolytica | 0.06 - 0.125|| Prevotella intermedia| ≤0.015 - 0.125|| Prevotella loescheii| 0.03 - 4|| Prevotella melaninogenica| 0.03 - 4|| Prevotella oris| 0.06 - 1|| Propionibacterium granulosum| <0.004|| Proteus mirabili| >100|| Proteus vulgaris| >100|| Providencia rettgeri| >100|| Pseudomonas aeruginosa | >100 - >4000|| Rhodococcus equi| ≤0.015 - >4|| Serratia marcescens| >100|| Staphylococci| 0.03 - 128|| Staphylococcus aureus| 0.03 - >128|| Staphylococcus epidermidis| <0.015 - >128|| Staphylococcus pneumonia| ≤0.03 - >512|| Staphylococcus saccharolyticus| 0.061|| Stenotrophomonas maltophilia| 8 - 64|| Streptococci| 0.001 - ≥64|| Streptococcus agalactiae| 0.008 - ≥32|| Streptococcus intermedius| <0.004|| Streptococcus pneumonia| 0.001 - >256|| Streptococcus pyogenes| 0.001 - >128|| Turicella otitidis| 0.03 - >128|| Ureaplasma spp.| ≤0.008 - 0.063|| Ureaplasma spp.| ≤0.008 - 0.5|| Ureaplasma urealyticum | ≤0.015 - 0.12|| Veillonella spp.| 1 - >32|| |